What is a resubmission code?
- A resubmission code is used to notify a carrier that the claim was either a corrected or replacement claim.
How do I add a resubmission code to my claim?
- To add a resubmission code to a claim, the claim would have to have been sent electronically at least one time and not have any payments associated with it.
- To activate this, you would select your patient and then click on Claim Correction Reprint.
- Highlight the claim in question and it will allow you to check off either Code 6 - Adjustment of Prior Electronic Claim or Code 7 - Replacement of a Prior Electronic Claim.
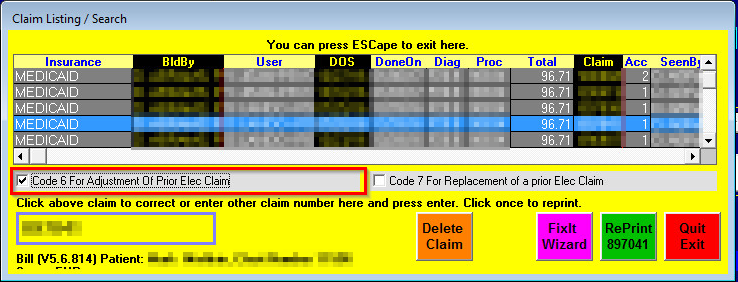
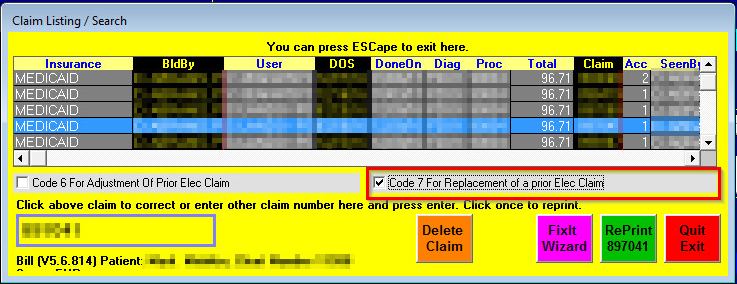
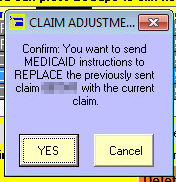
- After you select one of the two options you will receive a box asking if you would like to either replace or adjust the claim.
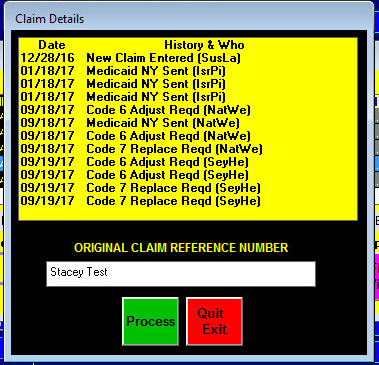
- After you say YES, you will be asked for the original claim reference number. This is located on the original EOB from the carrier and can be called CCN, ICN, etc. Enter the claim number and then select Process.
- Make the corrections that are need to the claim. Click Re-Process and then select Yes to Resubmit the claim.

- The claim history will show the Code which code was used . That the claim was corrected, and if it was added to the future listing (2Go=Insurance).

Can I use a resubmission code on partially paid claims?
- No, a resubmission code can only be used on a claim without any payments.
Is it possible to add a resubmission code to a secondary or tertiary claim?
- No, a resubmission code can only be used on the primary insurance.
Can I add Resubmission codes for a paper claim?
- You can add resbmission codes to a paper claim in the Reprints area
- This information may be added to primary, secondary or tertiary claims.
- The information you add is not saved or stored, so if you use this feature it is highly recommended that you maintain a copy after printing it. (Scan and save a copy in the patients filing cabinet)
- Open claim "Claim Corr/Rprnt" button on the patient chart screen.
- Select the claim you wish to print (click once to select it).
- Click the green "Reprint" option.
- If your claim is a seondary or tertiary claim, click the correct button ( Print Secondary/Tertiary HCFA Form)
- On the menu options at the top, Click on "Other Tasks" and select "Insert Carrier Resubmission Code and Ref Number"

6. Enter the required Resubmission code 6 (Adjustment of a prior claim) or 7 (Replacement of a previous claim) .
*Although this says Medicaid, it will work for any carrier

7. Enter the Originial Claim (Reference number).

8. You will see the information added to the form.
 '
'
9. Print the claim
