CMS Medicare changed the way they are handling secondary claims which is causing claims to be rejected due to missing Insurance type codes when patients are not typical Medicare beneficiaries. Below are samples of two common Medicare eligibility results that will assist you in determining what code is needed on the claim.
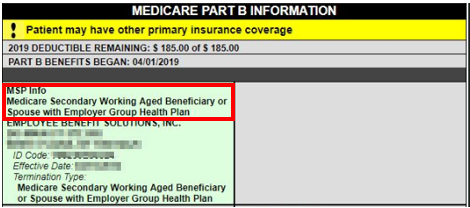
This result indicates the patient is 65 and over and is still working so it has other primary insurance with Medicare as a secondary. This type of patient will need the billing code of 12 on their claims.
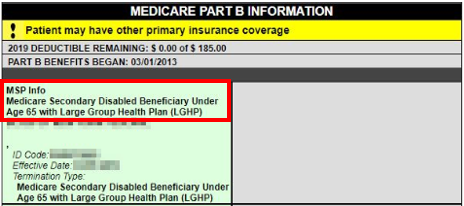
The eligibility result below means the client is under 65 but has Medicare disability benefits. Their claims require the use of code 43.
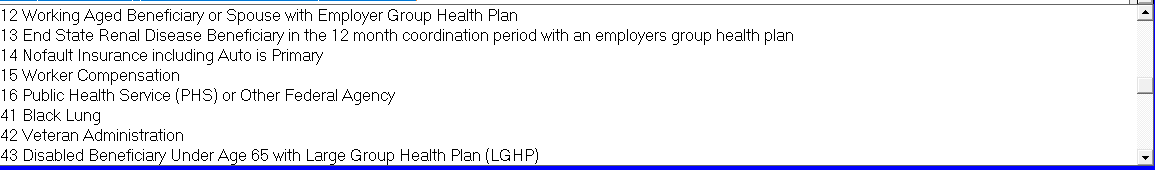
Other Medicare billing codes:
When checking eligibility different results may be returned which may indicate you need to choose an Insurance type code when billing. Below is the full list of Insurance type codes you may need to use depending on the Medicare eligibility results.

How to include the codes on claims:
You can access this list to include the code on the claim from the billing screen and click on the button Other Info. Click the drop down menu labelled Primary Insurance Type Code When Secondary Is Electronic
How to fix claims that were are already submitted and now rejected:
If you already posted the payment from the primary you will need to do the following steps to correct the claim to resubmit:
- Check the patient’s Medicare eligibility by clicking the eligibility button on the patient chart.
- Reverse the payments that were posted on the claim. You will need to re-post these payments so make sure you have either the EOB or a screenshot to assist in re-posting the claim correctly.
- Claim correct the claim and click the button other info and choose the appropriate Insurance type code.
- Re-post the payment from the primary.
Resubmit the claim to Medicare.
